
Post by : Anis Karim
Diabetes has long been a challenging condition, affecting millions worldwide. Type 1 diabetes, in particular, requires lifelong insulin therapy due to the autoimmune destruction of insulin-producing beta cells in the pancreas. However, a groundbreaking medical development offers new hope. For the first time, CRISPR-edited pancreas cells have been successfully implanted into a patient with type 1 diabetes, producing insulin without triggering immune rejection. This milestone represents a major step toward a potential cure for the disease and could transform the lives of millions who depend on insulin injections daily.
CRISPR-Cas9 technology has already revolutionized genetic research over the past decade. Its precision in editing genes has enabled scientists to correct genetic defects and enhance cellular functions. In this latest study, researchers used CRISPR to modify donor pancreatic islet cells. These modifications allowed the cells to evade the recipient’s immune system, preventing the typical immune attacks that destroy insulin-producing cells. Unlike traditional transplants that require immunosuppressive drugs to avoid rejection, this approach minimizes the need for such medications, reducing associated health risks.
The process begins with donor islet cells obtained from healthy pancreatic tissue. These cells are then genetically engineered using CRISPR to silence specific genes that would typically trigger an immune response. Additionally, researchers included modifications to make the cells more resistant to autoimmune attacks, which are the primary cause of beta-cell destruction in type 1 diabetes.
Once prepared, the cells were implanted into the patient’s forearm muscles, rather than the traditional site in the liver. This approach allows better monitoring and reduces potential complications. Within 28 days, the patient’s body began producing insulin effectively, demonstrating that the cells could function normally outside their original pancreatic environment.
What sets this achievement apart is the absence of immune suppression. Previous attempts at islet cell transplantation required lifelong immunosuppressive therapy, which comes with serious side effects, including increased infection risk and organ damage. By eliminating the need for these drugs, CRISPR-edited cells could dramatically improve quality of life for patients and make the therapy more widely accessible.
Type 1 diabetes affects an estimated 1.6 million Americans alone, with millions more worldwide. Currently, patients manage their condition through a combination of insulin injections, blood sugar monitoring, and careful diet and lifestyle choices. Despite advancements in insulin delivery and continuous glucose monitoring, the condition remains a heavy burden.
A successful CRISPR-based therapy could relieve this burden by offering a curative approach rather than lifelong management. Patients might eventually avoid daily injections, glucose monitoring, and complications such as kidney damage, neuropathy, and cardiovascular disease. Moreover, the therapy could reduce healthcare costs over time, as hospitalizations and long-term complications decrease.
Experts emphasize that while the initial results are promising, broader clinical trials are necessary. Long-term studies will need to assess how long the edited cells can survive and function, whether there are unforeseen side effects, and how different patient populations respond to the therapy. Nonetheless, this breakthrough represents a historic step forward, bridging the gap between experimental genetic therapy and practical clinical application.
Despite the excitement surrounding CRISPR therapies, several challenges remain. First, the long-term safety of gene-edited cells is unknown. While initial results are positive, unforeseen complications could emerge months or years after implantation. Researchers must also ensure that off-target gene edits—unintended changes in other parts of the genome—are minimized to prevent potential health risks.
Ethical concerns also come into play. Gene editing in humans, even when limited to therapeutic interventions, raises questions about access, consent, and long-term societal impact. Should such treatments be available only to those who can afford them? Could disparities in access worsen existing health inequalities? These questions highlight the need for careful regulation and ethical oversight as the technology progresses.
Additionally, scalability is a critical consideration. Producing CRISPR-edited cells is complex and resource-intensive. For this therapy to benefit millions of patients globally, researchers will need to develop cost-effective and efficient production methods. Collaborations between academic institutions, biotech companies, and regulatory bodies will be crucial to bring this therapy from small-scale trials to widespread use.
The success of CRISPR-edited cells in diabetes therapy is just one example of how gene editing is transforming medicine. CRISPR has shown promise in treating genetic disorders such as sickle cell anemia, muscular dystrophy, and certain types of inherited blindness. Its precision allows scientists to target disease-causing genes directly, potentially offering cures rather than symptom management.
In diabetes specifically, CRISPR opens the door to several innovative strategies beyond cell transplantation. Researchers are exploring ways to repair patients’ own pancreatic cells, enhance insulin production, and even develop “smart” cells that respond dynamically to blood sugar levels. These innovations could redefine chronic disease management in the coming decades.
The implications of CRISPR-based diabetes therapy extend far beyond a single patient or country. If proven safe and effective on a large scale, this approach could set a precedent for treating other autoimmune diseases, such as multiple sclerosis or lupus, by protecting vulnerable cells from immune attack. The global healthcare landscape could shift dramatically, with gene-editing therapies becoming a central component of chronic disease treatment.
Governments, healthcare providers, and biotech companies are already taking notice. Investment in CRISPR research is growing, regulatory frameworks are evolving, and public awareness is increasing. As the technology matures, it will be essential to balance innovation with ethical responsibility and equitable access.
The successful implantation of CRISPR-edited pancreas cells in a patient with type 1 diabetes represents a historic milestone in medical science. By producing insulin without triggering immune rejection, this breakthrough offers hope for a future where diabetes can be effectively cured rather than managed. While challenges remain, including long-term safety, ethical considerations, and scalability, the potential benefits are transformative.
CRISPR therapy has the power to redefine chronic disease treatment, not only for diabetes but for a range of autoimmune and genetic disorders. With careful research, regulation, and global collaboration, this technology could usher in a new era of medicine, offering millions of patients the chance for a healthier, insulin-free life.
This article is for informational purposes only and does not constitute medical advice. Patients should consult qualified h

Winter Skin Care: 10 Hydrating Drinks That Give Natural Glass Skin Glow
Learn how simple winter drinks keep your skin hydrated reduce dryness and support a natural glass sk

10 Songs That Carry the Same Grit and Realness as Banda Kaam Ka by Chaar Diwari
From underground hip hop to introspective rap here are ten songs that carry the same gritty realisti

PPG and JAFZA Launch Major Tree-Planting Drive for Sustainability
PPG teams up with JAFZA to plant 500 native trees, enhancing green spaces, biodiversity, and air qua

Dubai Welcomes Russia’s Largest Plastic Surgery Team
Russia’s largest plastic surgery team launches a new hub at Fayy Health, bringing world-class aesthe
The Art of Negotiation
Negotiation is more than deal making. It is a life skill that shapes business success leadership dec

Hong Kong Dragon Boat Challenge 2026 Makes Global Debut in Dubai
Dubai successfully hosted the world’s first Hong Kong dragon boat races of 2026, blending sport, cul

Ghanem Launches Regulated Fractional Property Ownership in KSA
Ghanem introduces regulated fractional real estate ownership in Saudi Arabia under REGA Sandbox, ena

Winter Skin Care: 10 Hydrating Drinks That Give Natural Glass Skin Glow
Learn how simple winter drinks keep your skin hydrated reduce dryness and support a natural glass sk

Why Drinking Soaked Chia Seeds Water With Lemon and Honey Before Breakfast Matters
Drinking soaked chia seeds water with lemon and honey before breakfast may support digestion hydrati

Morning Walk vs Evening Walk: Which Helps You Lose More Weight?
Morning or evening walk Learn how both help with weight loss and which walking time suits your body

What Really Happens When You Drink Lemon Turmeric Water Daily
Discover what happens to your body when you drink lemon turmeric water daily including digestion imm
DXB News Network Presents “Ctrl+Alt+Wim”, A Bold New Satirical Series Starring Global Entertainer Wim Hoste
DXB News Network premieres Ctrl+Alt+Wim, a bold new satirical micro‑series starring global entertain

High Heart Rate? 10 Common Causes and 10 Natural Ways to Lower It
Learn why heart rate rises and how to lower it naturally with simple habits healthy food calm routin

10 Simple Natural Remedies That Bring Out Your Skin’s Natural Glow
Discover simple natural remedies for glowing skin Easy daily habits clean care and healthy living ti
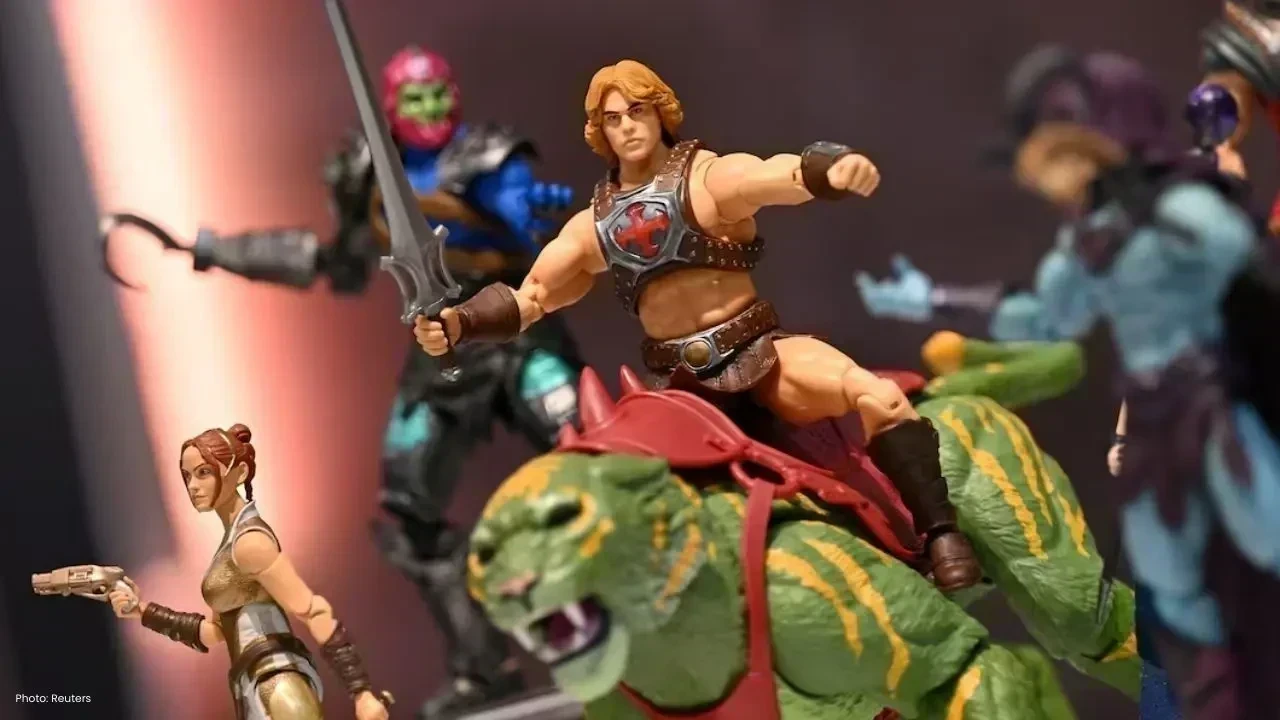
Mattel Revamps Masters of the Universe Action Figures for Upcoming Film
Mattel is set to revive Masters of the Universe action figures in sync with their new movie, ignitin